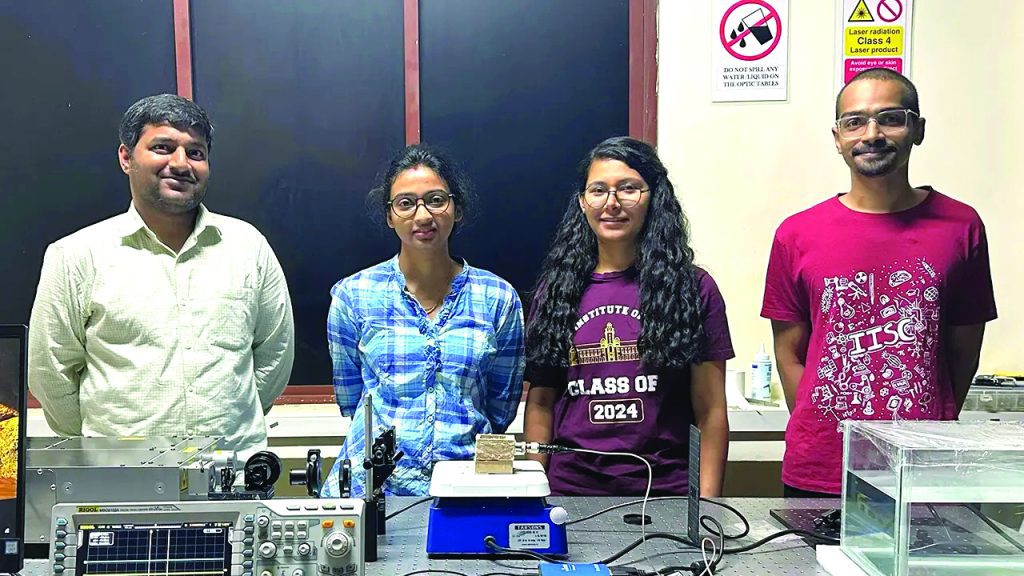
Image Courtesy: IISc
TECH TALK
In a significant breakthrough that could change the way diabetes is managed, scientists at the Indian Institute of Science (IISc), Bengaluru, have developed a new method for monitoring blood glucose levels—without the need for painful finger pricks or invasive sensors.
Using photoacoustic sensing, the team has demonstrated how light and sound can be used to estimate glucose concentrations in the body non-invasively. The study, published in Science Advances, marks a promising step towards painless, portable glucose monitoring devices for daily use.
“For people with diabetes, frequent blood sugar testing is essential, but the current methods are invasive and inconvenient,” said Dr Jaya Prakash, Assistant Professor at IISc’s Department of Instrumentation and Applied Physics, and lead author of the study, in a press release issued by IISc. “Our approach could eliminate the need for drawing blood entirely.”
HOW THE TECHNOLOGY WORKS
The core of the innovation lies in using laser pulses to generate subtle sound waves inside the body. When laser light is absorbed by biological tissue, it causes a minute rise in temperature, leading to slight expansion. This expansion produces vibrations that emit sound waves—a phenomenon known as the photoacoustic effect.
The researchers discovered that glucose molecules alter the intensity of these sound waves. By measuring this acoustic signal, they were able to estimate blood sugar levels with near-clinical accuracy, without piercing the skin.
Moreover, glucose is a chiral molecule, meaning it can rotate polarised light. This rotation also affects the strength of the photoacoustic signal, offering an additional method of glucose detection. “We’ve established a clear relationship between glucose concentration and the acoustic signal intensity at specific wavelengths,” Dr Prakash added.
FROM LAB TO HUMAN TESTING
The team first tested the method on glucose-mixed water and serum solutions, followed by trials on animal tissue. Encouraged by the results, it then conducted a pilot study on a human participant, monitoring blood sugar changes before and after meals over three days. The technology successfully tracked glucose fluctuations, proving its potential for real-world use.
Another significant advantage of the method is its ability to take readings at varying tissue depths. “Unlike light, sound waves don’t scatter much inside the body, so we obtained reliable measurements at different layers,” said Swathi Padmanabhan, a PhD student at IISc and first author of the study.
Despite the success, the technology is not yet ready for commercial rollout. The current system uses high-end nanosecond-pulse lasers that are expensive and bulky. “Our next goal is to develop a compact and affordable version of this setup,” Padmanabhan said. “Miniaturisation will be key to bringing this to clinics and homes.”
The team believes that its technique could have far-reaching applications. Since many drugs — including naproxen, a commonly used painkiller — are also chiral, the same approach could be used to detect them in the body.
“With the right wavelength of light, this method could potentially detect various chiral compounds,” Dr Prakash explained. “This opens new avenues in diagnostics and drug monitoring.”
The IISc study could revolutionise diabetes care by making blood sugar tracking painless, faster, and more accessible. If the system can be made portable and cost-effective, it may replace the conventional glucometer.